Advice
Tags

MD vs PA: What are the Differences and Similarities
Are you someone who can’t decide between becoming a medical doctor or a physician assistant? You’re not alone! Many students are on the same boat of uncertainty.
To help you decide, we’ve outlined the key differences between the two professions in terms of education, job responsibilities, salary, and lifestyle. This way, you can make an informed decision that’s best for you.
EDUCATION
Although both medical doctors (MD) and physician assistants (PA) are qualified medical professionals, the level of education they receive varies drastically.
The path towards becoming an MD is much longer compared to becoming a PA. It’s a very lengthy process, with several years of schooling and specialized training.
As an MD, you must complete 6-12 years of education following an undergraduate degree:
- 3-4 years of medical school
- 2-5 years of residency, depending on your program of choice/the program you are matched with
- 1-2 additional years if you choose to further specialize and complete a fellowship
On the other hand, becoming a PA only requires an additional couple of years following undergraduate studies. After two years of Physician Assistant School, and once you have written and passed the certification exam, you can directly apply for a staff position.
PAs and MDs are both trained under the Medical Model of health, which aims to identify disease through a systematic process of observation, in accordance with standard procedure. However, MDs hold more in-depth knowledge of medical topics since the curriculum of PA school is more compressed. Regardless, since they follow the same Medical Model, both professions are taught to think, learn and practice in the same way, helping them work extremely well together.
As you’ll learn next, PAs and MDs work closely alongside and complement each other’s responsibilities.
SKILLS & RESPONSIBILITIES
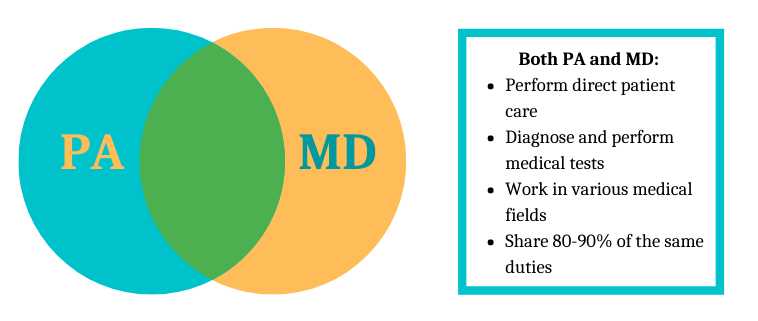
When it comes to the duties and responsibilities of MDs and PAs, there’s a high degree of overlap. For example, both professions involve direct patient care, both are able to work in a specialized field or setting, and both are regulated professions in their own right. The two professions work collaboratively together to ensure efficiency, effective treatment delivery, and the highest degree of patient care.
There are also several factors related to job responsibilities that clearly differentiate the two professions.
Medical doctors are independent practitioners who have full liability over their patients. They are directly assigned their own list of patients, are able to open their own practice, and have a variety of privileges in clinics and hospital settings, including in specialized fields such as surgery. They can also make medical diagnoses and prescribe medication.
In contrast, PAs are not independent medical professionals; they always work with a supervising physician who delegates tasks to them. Though PAs can usually perform the majority of the work that the physician can, they are unable to complete a task that is not delegated to them.
In some cases, the supervising MD offloads simpler tasks onto the PA in order to focus on more complex or specialized tasks they’ve been trained for. In the majority of cases, however, PAs are able to perform ~80-90% of the duties of an MD; they can diagnose and treat illness, perform medical tests and exams, advise patients on recommended steps, and prescribe medication, to name a few.
It is also important to remember that a PA is unable to perform a task that their supervising MD is unable to perform themselves – their tasks depend on their supervising physician’s scope of practice. This rule still applies if the PA holds a skill from a previous role working with a different supervising physician. While it may seem unreasonable, it ensures optimal patient safety and reduces liability for the supervising physician who may not hold that particular skill.
One way to look at it is that a PA is an ‘extension’ of the supervising physician, signifying their fundamental role in the medical field. It’s important to recognize that both professions are crucial to the healthcare process; one is not superior over the other.
SALARY
Though the average salary for an MD in Ontario is quite high (family doctors make an average of around $300,000 per year), you should keep in mind that they start off as residents, making around $51,000 per year. Depending on the length of their program, residents may be relying on this salary for several years, which may make it difficult for anyone who has to pay medical student debt as well as afford a comfortable standard of living.
As well, for a physician who chooses to open their own practice, there are several budgetary factors to consider, including rent, staff salaries, and up-to-date medical equipment. Practice owners usually also have to take care of their own work benefits whereas PAs, as employees, are able to take advantage of benefits provided to them.
The starting salary for a PA is an average of $75,000 a year, which is definitely more comfortable than a resident salary. Like in many professions, the salary of a PA can grow with skill and experience. It can also depend on the field of medicine that a PA chooses to practice in; for instance, working in occupational medicine or the critical care unit of a hospital usually pays more than a position at a university health clinic or a nursing home.
While the pay of a PA may be lower than that of an MD, it’s still a very reasonable salary that can help you live comfortably. What you end up deciding really all depends on your goals and priorities. In the next section, we’ll discuss important lifestyle differences between the two professions that may help you make this important decision.
 LIFESTYLE: WORK-LIFE BALANCE
LIFESTYLE: WORK-LIFE BALANCE
PAs enjoy a high degree of flexibility when it comes to how many hours they work and under what conditions. For example, their contracts could explicitly indicate that they opt not to work overnight or on-call shifts, or even other conditions depending on the practice. Of course, they could similarly opt to work those shifts if they choose to.
Essentially, there is lots of room for PAs to choose how to manage a work-life balance that works best for them. In this way, they can better avoid becoming overwhelmed or burnt out. On the contrary, job dissatisfaction and burnout are issues faced by many MDs because of the high intensity and level of requirements of many specialities.
PAs also enjoy flexibility when it comes to changing their area of practice. If a PA wants to switch their specialization, they do not have to undergo any additional schooling or certification. Remember, the role of a PA is closely tied to the scope of practice of their supervising physician. If there are skills that are very specific to a certain area of medicine, the physician will work with the PA to build those necessary skills.
When it comes to the lifestyle of an MD, it really depends on the speciality that you practice in. An emergency room physician might have a less flexible schedule than an ophthalmologist or family doctor. The latter two specialties generally have a set schedule, with the exception of physicians who work in a hospital setting and therefore might be required to work an on-call shift every few weeks.
Generally speaking, however, physicians can still enjoy a work-life balance that best suits them. For instance, although an emergency room physician may be required to work an exhaustive schedule, they also tend to have more days off compared to other specialties. They can typically take their days off back-to-back, allowing them to travel, recuperate, and catch up on other personal and family matters.
However, keep in mind that before you finish your specialty training and while you’re still a resident, you might see very little flexibility in your work-life balance. Residents are generally known to be overworked and underpaid, so there’s a lot of road to tread before landing a pristine schedule with set hours and secured leisure time.
When it comes to switching areas of practice, an MD must generally complete years of additional training for certification in the newly chosen field, especially with more technical fields like ophthalmology or general surgery.
MAKING YOUR DECISION
When deciding which path is best for you, make sure to consider every factor. Understand what it is you are looking for in a career, what type of work-life balance you want to achieve, and what you want your life to look like in the future.
If you’re having trouble, shining a unique light on your application, or structuring your writing well, don’t hesitate to get in touch with us. Our talented team of experts is always happy to help.
